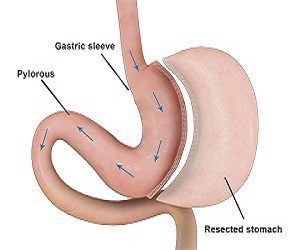
Vertical sleeve gastrectomy is a restrictive form of weight loss surgery in which approximately 75% of the stomach is removed leaving a cylindrical or sleeve-shaped stomach with a capacity ranging from about 60 to 150 cc, depending upon the surgeon performing the procedure. Unlike many other forms of bariatric surgery, the outlet valve and the nerves to the stomach remain intact, and while the stomach is drastically reduced in size, its function is preserved. Again, unlike other forms of surgery such as the Roux-en-Y gastric bypass, the sleeve gastrectomy is not reversible.
Because the new stomach continues to function normally there are fewer restrictions on the foods that patients can consume after surgery, albeit that the quantity of food eaten will be considerably reduced. This is seen by many patients as being one of the great advantages of the sleeve gastrectomy, as is the fact that the removal of the majority of the stomach also results in the virtual elimination of hormones produced within the stomach which stimulate hunger.
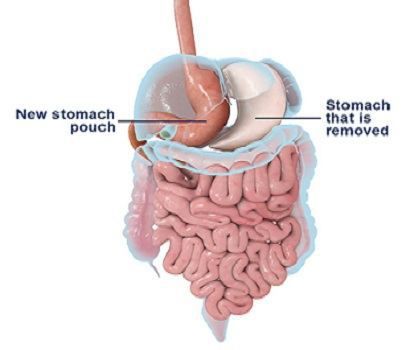
Perhaps the greatest advantage of the gastric sleeve lies in the fact that it does not involve any bypass of the intestinal tract and patients do not therefore suffer the complications of intestinal bypass such as intestinal obstruction, anemia, osteoporosis, vitamin deficiency and protein deficiency. It also makes it a suitable form of surgery for patients who are already suffering from anemia, Crohn’s disease and a variety of other conditions that would place them at a high risk for surgery involving intestinal bypass.
Finally, it is one of the few forms of surgery which can be performed laparoscopically in patients who are extremely overweight, and this accounts for the rising popularity of the laparoscopic sleeve gastrectomy.
Perhaps the main disadvantage of this form of surgery is that it does not always produce the reduction in weight which people would wish for, and in the longer term, can result in weight regain. This is indeed true of any form of purely restrictive surgery, but is perhaps especially true in the case of sleeve gastrectomy.
Because the procedure requires stapling of the stomach, patients do run the risk of leakage and of other complications directly related to stapling. In addition, as with any surgery, patients run the risk of additional complications such as post-operative bleeding, small bowel obstruction, pneumonia and even death.
The risk of encountering any of these complications is however extremely small and varies from about 0.5 to 1%. Having said this, the risk of death from this form of surgery at about 0 .25% is extremely small.
As a general rule the vertical sleeve gastrectomy is best suited to individuals who are either extremely overweight or whose medical condition would rule out other forms of surgery. In the case of the former, vertical sleeve gastrectomy would normally form the first of a two-part surgical plan, with further bariatric surgery being performed once the patient’s weight has fallen sufficiently to allow for other forms of surgery to come into play.
Alternative names: Vertical sleeve gastrectomy, sleeve gastrectomy, greater curvature gastrectomy, parietal gastrectomy, gastric reduction and vertical gastroplasty.
Surgery for high BMI patients: For patients with a particularly high body mass index (typically 50+) many forms of weight loss surgery are either difficult to perform or present increased risk. As a result, a vertical sleeve gastrectomy (or increasingly a laparoscopic sleeve gastrectomy) is sometimes performed as the first of a two-part weight loss solution to provide an initial drop in weight which then makes other bariatric follow up possible at a reduced level of risk.
Surgery for low BMI patients: For obese patients with a relatively low body mass index the vertical sleeve gastrectomy can also prove a good choice, especially where existing conditions (such as anemia or Crohn’s disease) prevent them from having other forms of bariatric surgery. In addition, patients may choose this form of surgery if they are concerned about the long-term effects of bypass surgery or object to having a ‘foreign’ body implanted into their body, as is the case with lap band surgery.
The Ghrelin effect: An additional effect is that removing 90% of the stomach reduces the amount of the hunger hormone Ghrelin that is produced; so for the first 6 months most sleeve patients notice a significant reduction in hunger and appetite, even when hunger does start.
No adjustments required: It is ideal for patients who live or work in remote areas because no post-operative adjustments are possible or required. There is also no risk of food getting stuck on the LAGB.
Improved quality of eating: Unlike the band and gastric bypass, there is no outlet restriction so patients can eat just about whatever type of food, just much smaller amounts. Vomiting is much less frequent than after a band and is uncommon after a few months when you get used to the new capacity of your stomach. Typically, an entree size portion feels like a banquet.
Superior weight loss vs. LAGB: The weight loss with the sleeve is more rapid than a band and approaches that of a bypass, being 70-80 % by one year (based on a 36 fr sleeve) and 65% by three years (based on 40 fr sleeve). The sleeve does stretch up a little over time.
If there were to be significant weight regain, the sleeve can be further reduced by resleeving, or a band placed around the sleeve or a bypass created from it.
Good revision option: It might also be a good option if patients have a problem with their band requiring revision, have already lost a lot of weight and don’t want a full bypass. It is our preferred revision option for all failed bands. We have found, however that if patients already have a band, the safest sequence is to first remove the band and prepare the stomach wall, then wait three months before sleeving. This minimizes the risk of leak and other complications.
As with all forms of weight loss surgery, the vertical gastrectomy does carry risks, and these will clearly vary from one patient to the next and must be discussed with your physician. Complications might include: